You Had One Job… 
‘If you were Chief Nursing Officer for the day – what would you do?’
It’s a question I sometimes ask groups of nurses & midwives when I manage to engage them in conversation. The answers vary greatly – and tend to be person specific. I’m also keen to know what the one thing is that either stops nurses and midwives from doing a great job, or what one thing would make it easier for them to do a great job; again the answers are variable.
 The launch of the Nursing Vision 2030 http://www.gov.scot/Publications/2017/07/4277/6 in July was essentially a compilation of people’s thoughts, hopes and dreams for how we support the profession to move forwards. So for me making good progress on implementing the Vision would certainly be one thing for me to do in the coming year.
The launch of the Nursing Vision 2030 http://www.gov.scot/Publications/2017/07/4277/6 in July was essentially a compilation of people’s thoughts, hopes and dreams for how we support the profession to move forwards. So for me making good progress on implementing the Vision would certainly be one thing for me to do in the coming year.
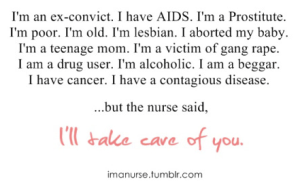
Supporting nurses to deliver personalised care in a compassionate and caring way is an easy thing to say, but much more complex to do, and the Vision sets out the direction of travel for the profession. The three themes of:
- Personalising Care,
- Preparing Nurses for the Future and
- Supporting Nurses
are interwoven in the Vision but set out clearly where we need to get to.
And whilst I know that more nurses is not always the answer to supporting the delivery of excellence in care, I recognise that without the right numbers of staff, with the right skills, high quality care is unlikely to be delivered. So the government’s ambition to increase the numbers of student nurses and midwives by 2600 in this parliament is welcome.
 At the time of writing, the Cabinet Secretary had yet to announce the figures for student nurse and midwifery intakes for 2018/19, but at the moment, there have been five successive years where intakes have increased.
At the time of writing, the Cabinet Secretary had yet to announce the figures for student nurse and midwifery intakes for 2018/19, but at the moment, there have been five successive years where intakes have increased.
Widening Access
However we need to do more than our traditional way of increasing numbers of intakes into year one of our education programmes. I’ve seen how important it is to support our HCSWs into nursing, and fretted about how to support people into nursing who may not have been our traditional go to people to come into the profession. Which is why I commissioned Professor Paul Martin to look at widening participation in nursing & midwifery education and careers. I had hoped that through Paul’s leadership we could have solid advice around how we build on what we currently do well, and I certainly wasn’t disappointed: http://www.gov.scot/Resource/0052/00528586.pdf
 The Commission was published in early December and has some challenging recommendations, which I’m confident will stand the professions in good stead in the years to come. It will open up the professions in many ways; both by supporting people into higher education who may not have traditionally studied at that level, and also by attracting people into the professions who are already graduates and are looking for a change.
The Commission was published in early December and has some challenging recommendations, which I’m confident will stand the professions in good stead in the years to come. It will open up the professions in many ways; both by supporting people into higher education who may not have traditionally studied at that level, and also by attracting people into the professions who are already graduates and are looking for a change.
Notably, there is significant work to be done in our Care Home settings – where the opportunity for professional growth and development is undervalued.
Looking back then on last year, in preparation for looking forwards, we’ve much to celebrate; preparation for our employer led midwifery supervision programme was launched and has been well received; our work on transforming roles is helping the professions to flex and change so that we can continue to support health improvement and deliver care, across a range of settings; and the work on safe staffing, whilst at times challenging, is moving forwards and will support the delivery of Excellence in Care – our improvement and assurance approach for nursing and midwifery care across Scotland.
2018
 From a service level perspective, regional plans are being developed, health and social care continues to integrate, and the Best Start has been launched- which is a real opportunity for midwives to support the next generation into better health.
From a service level perspective, regional plans are being developed, health and social care continues to integrate, and the Best Start has been launched- which is a real opportunity for midwives to support the next generation into better health.
However, if there is one job for me next year, it’s taking steps to support the improvement of the health of Scotland’s nurses and midwives. In our consultation for the Vision, nurses themselves signalled that at times, challenges with their personal health and wellbeing got in the way of delivering the care they would want to deliver. I know that there is an emotional cost of caring that is challenging for our professions – a bitter sweet aspect of our practice – it’s what has often drawn us into the profession and makes it so special, but if not carefully managed, can cause burnout.
And as we age (gracefully I hope) our physical health at times can also take its toll. Figures published earlier in the year highlight that the public health problem of obesity has left its mark on nurses and midwives – who suffer from obesity to a greater extent than the rest of the population. So as I step forwards into a new year with new challenges, health and wellbeing of the profession will be at the top of my list.
This blog was written by Professor Fiona C McQueen (@fionacmcqueen), Chief Nursing Officer for Scotland at the Scottish Government.
Post Script 31 December 2017, 19:00hrs.
Readers of this blog are most likely to be aware of how busy our services have been over the holiday period. My Scottish Government Director colleagues, and others have been monitoring activity across Scotland, which has been higher than we would have expected. Whilst we’ll have to wait for ‘official’ statistics, services across Scotland are reporting people presenting with flu as well as other illnesses, which has been putting greater pressure than usual on our services. A number of us have been visiting sites to be with staff as they continue to deliver care to their patients.
 This morning I had the pleasure of visiting Ayr Hospital. On arriving at the main entrance, Kieran, one of the domestic team was taking a great pride in keeping the hospital spotless. I was blown away by his enthusiasm and pride for his job.
This morning I had the pleasure of visiting Ayr Hospital. On arriving at the main entrance, Kieran, one of the domestic team was taking a great pride in keeping the hospital spotless. I was blown away by his enthusiasm and pride for his job.
Visiting ED, ITU, the assessment unit as well as a number of wards, I was left in no doubt of the professionalism and dedication of the whole team; I met nurses, doctors, AHPs and others – all giving of their best and taking a real pride in their work.
Entering a new year, I have no doubt the staff of NHS Scotland are the life blood of our service, and our soon to be 70 year old NHS is very safe in their hands.








 1. Cycling is better than running, however, turns out the kit can be ridiculously expensive (but it’s worth it for the reversible green and black cycling jacket and the fancy reflective tabs on my cycling trousers….)
1. Cycling is better than running, however, turns out the kit can be ridiculously expensive (but it’s worth it for the reversible green and black cycling jacket and the fancy reflective tabs on my cycling trousers….) 3. We have outgrown the Breakthrough Collaborative method for our more mature improvement work, so we have had to think differently:
3. We have outgrown the Breakthrough Collaborative method for our more mature improvement work, so we have had to think differently:
 4. The iPhone 7+ is way better than the 6+ because I can now take it swimming and the phone would survive (unlike the blackberry….long story)
4. The iPhone 7+ is way better than the 6+ because I can now take it swimming and the phone would survive (unlike the blackberry….long story)
 6. How about this for a statistic? 73% of the UK population defines the NHS as the quintessential feature that made them proud to be British
6. How about this for a statistic? 73% of the UK population defines the NHS as the quintessential feature that made them proud to be British
 9. An acting coach is not as bad as she sounds – she taught me to get better at storytelling for “What Matters to Me: a new vital sign” for TEDx Glasgow in June.
9. An acting coach is not as bad as she sounds – she taught me to get better at storytelling for “What Matters to Me: a new vital sign” for TEDx Glasgow in June.  And talking of What Matters To Me, I learnt that “What Matters To You Day” on June 6th 2016 attracted 500 health systems and 11 countries to take part – a fantastic achievement for everyone involved.
And talking of What Matters To Me, I learnt that “What Matters To You Day” on June 6th 2016 attracted 500 health systems and 11 countries to take part – a fantastic achievement for everyone involved.
 After four years of posting a blog every week come rain, shine and holidays, leading to 215 blog posts, Ayrshirehealth blog is coming to an end – it is a situation of mixed emotions and necessitates some important thank yous.
After four years of posting a blog every week come rain, shine and holidays, leading to 215 blog posts, Ayrshirehealth blog is coming to an end – it is a situation of mixed emotions and necessitates some important thank yous.

 After 32 years in the NHS I am leaving to take on a new opportunity (@dtbarron) – this time, just like the NHS, with another much loved organisation – Erskine, the veterans charity, where I’ll be privileged to take up the post as Director of Care.
After 32 years in the NHS I am leaving to take on a new opportunity (@dtbarron) – this time, just like the NHS, with another much loved organisation – Erskine, the veterans charity, where I’ll be privileged to take up the post as Director of Care.
 If you are thinking of starting your own blog – consider adopting Stephen Covey’s second habit “Begin with the end in mind” remembering, if you don’t know where you want to go, then any road will take you there:
If you are thinking of starting your own blog – consider adopting Stephen Covey’s second habit “Begin with the end in mind” remembering, if you don’t know where you want to go, then any road will take you there:













 Information and health was recognised as an important enabler, both in terms of sharing information across and within teams, but also in reducing administrative aspects of the nurses role. There was a clear enthusiasm evident from those present.
Information and health was recognised as an important enabler, both in terms of sharing information across and within teams, but also in reducing administrative aspects of the nurses role. There was a clear enthusiasm evident from those present.

















 In a few months time I have the important job of completing
In a few months time I have the important job of completing 









 The main message is that Library Services saves clinicians time and provides them with up-to-date information to inform their practice. Promotion of the service and the resources available to staff and students is a constant part of my role.
The main message is that Library Services saves clinicians time and provides them with up-to-date information to inform their practice. Promotion of the service and the resources available to staff and students is a constant part of my role.



